How Do You Know Youre Dying From Myasthenia Gravis
| Myasthenia gravis | |
|---|---|
 | |
| Eye difference and a drooping eyelid in a person with myasthenia gravis trying to open her optics | |
| Specialty | Neurology |
| Symptoms | Varying degrees muscle weakness, double vision, drooping eyelids, trouble talking, trouble walking[1] |
| Usual onset | Women nether twoscore, men over threescore[1] |
| Duration | Long term[1] |
| Causes | Autoimmune affliction[1] |
| Diagnostic method | Blood tests for specific antibodies, edrophonium test, nervus conduction studies[i] |
| Differential diagnosis | Guillain–Barré syndrome, botulism, organophosphate poisoning, brainstem stroke[2] |
| Treatment | Medications, surgical removal of the thymus, plasmapheresis[i] |
| Medication | Acetylcholinesterase inhibitors (neostigmine, pyridostigmine), immunosuppressants[1] |
| Frequency | l to 200 per million[iii] [4] |
Myasthenia gravis (MG) is a long-term neuromuscular disease that leads to varying degrees of skeletal muscle weakness.[1] The virtually commonly afflicted muscles are those of the eyes, face, and swallowing.[1] Information technology can issue in double vision, drooping eyelids, problem talking, and trouble walking.[1] Onset tin be sudden.[1] Those affected oftentimes have a large thymus or develop a thymoma.[1]
Myasthenia gravis is an autoimmune disease of the neuro-muscular junction which results from antibodies that block or destroy nicotinic acetylcholine receptors (AChR) at the junction betwixt the nerve and muscle.[5] [6] [ane] This prevents nerve impulses from triggering muscle contractions.[1] Virtually cases are due to immunoglobulin G1 (IgG1) and IgG3 antibodies that attack AChR in the postsynaptic membrane, causing complement-mediated damage and musculus weakness.[7] Rarely, an inherited genetic defect in the neuromuscular junction results in a similar condition known as congenital myasthenia.[8] [9] Babies of mothers with myasthenia may have symptoms during their first few months of life, known as neonatal myasthenia.[i] Diagnosis tin can exist supported by blood tests for specific antibodies, the edrophonium examination, or a nerve conduction report.[1]
MG is generally treated with medications known equally acetylcholinesterase inhibitors, such every bit neostigmine and pyridostigmine.[1] Immunosuppressants, such equally prednisone or azathioprine, may too exist used.[1] The surgical removal of the thymus may improve symptoms in certain cases.[ane] Plasmapheresis and loftier-dose intravenous immunoglobulin may be used during sudden flares of the condition.[one] If the breathing muscles become significantly weak, mechanical ventilation may be required.[1] One time intubated acetylcholinesterase inhibitors may be temporarily held to reduce airway secretions.[10]
MG affects l to 200 per meg people.[iii] [4] It is newly diagnosed in 3 to 30 per 1000000 people each year.[11] Diagnosis is becoming more common due to increased awareness.[11] MG most usually occurs in women under the age of 40 and in men over the age of lx.[i] Information technology is uncommon in children.[one] With treatment, most of those affected atomic number 82 relatively normal lives and have a normal life expectancy.[one] The word is from the Greek mys, "muscle" and astheneia "weakness", and the Latin gravis, "serious".[12]
Signs and symptoms
The initial, main symptom in MG is painless weakness of specific muscles, not fatigue.[13] The muscle weakness becomes progressively worse during periods of physical activeness and improves after periods of rest. Typically, the weakness and fatigue are worse toward the end of the day.[14] MG mostly starts with ocular (eye) weakness; information technology might then progress to a more severe generalized form, characterized by weakness in the extremities or in muscles that govern bones life functions.[fifteen]
Eyes
In about two-thirds of individuals, the initial symptom of MG is related to the muscles around the centre.[13] Eyelid drooping (ptosis may occur due to weakness of m. levator palpebrae superioris)[sixteen] and double vision (diplopia,[13] due to weakness of the extraocular muscles).[14] Heart symptoms tend to go worse when watching tv, reading, or driving, particularly in bright conditions.[13] Consequently, some affected individuals choose to wear sunglasses.[13] The term "ocular myasthenia gravis" describes a subtype of MG where muscle weakness is confined to the eyes, i.e. extraocular muscles, k. levator palpebrae superioris, and thou. orbicularis oculi.[xvi] Typically, this subtype evolves into generalized MG, unremarkably later a few years.[16]
Eating
The weakness of the muscles involved in swallowing may lead to swallowing difficulty (dysphagia). Typically, this means that some nutrient may be left in the mouth after an effort to swallow,[17] or food and liquids may regurgitate into the olfactory organ rather than go down the throat (velopharyngeal insufficiency).[xiv] Weakness of the muscles that motion the jaw (muscles of mastication) may cause difficulty chewing. In individuals with MG, chewing tends to become more tiring when chewing tough, fibrous foods.[13] Difficulty in swallowing, chewing, and speaking is the first symptom in about one-sixth of individuals.[13]
Speaking
Weakness of the muscles involved in speaking may lead to dysarthria and hypophonia.[13] Speech communication may be tiresome and slurred,[18] or have a nasal quality.[14] In some cases, a singing hobby or profession must be abandoned.[17]
Head and neck
Due to weakness of the muscles of facial expression and muscles of mastication, facial weakness may manifest equally the inability to hold the mouth closed[xiii] (the "hanging jaw sign") and every bit a snarling expression when attempting to smile.[fourteen] With drooping eyelids, facial weakness may brand the individual announced sleepy or sad.[13] Difficulty in holding the head upright may occur.[18]
Other
The muscles that control breathing and limb movements can also be affected; rarely do these present equally the first symptoms of MG, but develop over months to years.[19] In a myasthenic crisis, a paralysis of the respiratory muscles occurs, necessitating assisted ventilation to sustain life.[20] Crises may be triggered past various biological stressors such as infection, fever, an adverse reaction to medication, or emotional stress.[20]
Pathophysiology
MG is an autoimmune synaptopathy. The disorder occurs when the immune arrangement malfunctions and generates antibodies that attack the body's tissues. The antibodies in MG attack a normal human being protein, the nicotinic acetylcholine receptor, or a related protein chosen MuSK, a muscle-specific kinase.[21] Other, less frequent antibodies are found confronting LRP4, agrin, and titin proteins.[7] [22]
Man leukocyte antigen haplotypes are associated with increased susceptibility to myasthenia gravis and other autoimmune disorders. Relatives of people with myasthenia gravis have a higher percent of other immune disorders.[23] [24]
The thymus gland cells course part of the body's immune system. In those with myasthenia gravis, the thymus gland is large and aberrant. It sometimes contains clusters of allowed cells that betoken lymphoid hyperplasia, and the thymus gland may give wrong instructions to immune cells.[25]
-

-
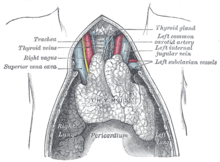
A juvenile thymus shrinks with historic period.
-

In pregnancy
For women who are pregnant and already accept MG, in a tertiary of cases, they accept been known to experience an exacerbation of their symptoms, and in those cases, it unremarkably occurs in the first trimester of pregnancy.[26] Signs and symptoms in significant mothers tend to improve during the second and third trimesters. Complete remission tin occur in some mothers.[27] Immunosuppressive therapy should exist maintained throughout pregnancy, as this reduces the chance of neonatal musculus weakness, and controls the female parent's myasthenia.[28]
Most 10–twenty% of infants with mothers affected by the status are built-in with transient neonatal myasthenia (TNM), which generally produces feeding and respiratory difficulties that develop near 12 hours to several days after birth.[26] [28] A child with TNM typically responds very well to acetylcholinesterase inhibitors, and the condition mostly resolves over a period of three weeks, as the antibodies diminish, and by and large does non result in whatsoever complications.[26] Very rarely, an infant can exist born with arthrogryposis multiplex congenita, secondary to profound intrauterine weakness. This is due to maternal antibodies that target an baby'south acetylcholine receptors. In some cases, the mother remains asymptomatic.[28]
Diagnosis
MG can be difficult to diagnose, equally the symptoms can be subtle and hard to distinguish from both normal variants and other neurological disorders.[17]
Three types of myasthenic symptoms in children tin exist distinguished:[29]
- Transient neonatal myasthenia occurs in ten to fifteen% of babies born to mothers affected with the disorder, and disappears later on a few weeks.
- Congenital myasthenia, the rarest grade, occurs when genes are present from both parents.
- Juvenile myasthenia gravis is most common in females.
Congenital myasthenias cause musculus weakness and fatigability similar to those of MG.[thirty] The signs of congenital myasthenia normally are nowadays in the showtime years of childhood, although they may not be recognized until machismo.[31]
Nomenclature
| Class | Description |
|---|---|
| I | Whatsoever middle muscle weakness, possible ptosis, no other evidence of muscle weakness elsewhere |
| Ii | Center musculus weakness of any severity, mild weakness of other muscles |
| IIa | Predominantly limb or axial muscles |
| IIb | Predominantly bulbar and/or respiratory muscles |
| Iii | Eye muscle weakness of whatsoever severity, moderate weakness of other muscles |
| IIIa | Predominantly limb or axial muscles |
| IIIb | Predominantly bulbar and/or respiratory muscles |
| Iv | Eye muscle weakness of whatever severity, severe weakness of other muscles |
| IVa | Predominantly limb or axial muscles |
| IVb | Predominantly bulbar and/or respiratory muscles |
| V | Intubation needed to maintain airway |
When diagnosed with MG, a person is assessed for his or her neurological status and the level of illness is established. This is usually washed using the accepted Myasthenia Gravis Foundation of America Clinical Nomenclature scale.[ citation needed ]
Concrete exam
During a physical exam to cheque for MG, a medico might enquire the person to perform repetitive movements. For example, the doctor may inquire 1 to look at a fixed signal for 30 seconds and to relax the muscles of the forehead, considering a person with MG and ptosis of the eyes might exist involuntarily using the forehead muscles to recoup for the weakness in the eyelids.[17] The clinical examiner might as well endeavour to arm-twist the "drape sign" in a person by holding ane of the person'due south eyes open, which in the example of MG will lead the other eye to shut.[17]
Blood tests
If the diagnosis is suspected, serology tin can be performed:
- One examination is for antibodies against the acetylcholine receptor;[17] the test has a reasonable sensitivity of 80–96%, but in ocular myasthenia, the sensitivity falls to 50%.
- A proportion of the people without antibodies against the acetylcholine receptor have antibodies confronting the MuSK poly peptide.[33]
- In specific situations, testing is performed for Lambert-Eaton syndrome.[34]
Electrodiagnostics

A chest CT-scan showing a thymoma (red circumvolve)

Photo of a person showing right partial ptosis (left pic), the left hat shows compensatory pseudo lid retraction because of equal innervation of the m. levator palpabrae superioris (Hering's constabulary of equal innervation): Correct picture: after an edrophonium exam, note the improvement in ptosis.
Musculus fibers of people with MG are easily fatigued, which the repetitive nerve stimulation test can aid diagnose. In unmarried-cobweb electromyography, which is considered to be the nigh sensitive (although not the near specific) test for MG,[17] a thin needle electrode is inserted into dissimilar areas of a particular muscle to record the action potentials from several samplings of different individual musculus fibers. Two muscle fibers belonging to the same motor unit are identified, and the temporal variability in their firing patterns is measured. Frequency and proportion of detail abnormal action potential patterns, called "jitter" and "blocking", are diagnostic. Jitter refers to the aberrant variation in the time interval betwixt action potentials of adjacent muscle fibers in the same motor unit. Blocking refers to the failure of nerve impulses to arm-twist action potentials in adjacent musculus fibers of the same motor unit of measurement.[35]
Ice test
Applying ice for 2–5 minutes to the muscles reportedly has a sensitivity and specificity of 76.nine% and 98.3%, respectively, for the identification of MG. Acetylcholinesterase is thought to be inhibited at the lower temperature, which is the basis for this diagnostic test. This generally is performed on the eyelids when ptosis is present and is deemed positive if a ≥2-mm ascent in the eyelid occurs after the ice is removed.[36]
Edrophonium examination
This exam requires the intravenous administration of edrophonium chloride or neostigmine, drugs that block the breakdown of acetylcholine by cholinesterase (acetylcholinesterase inhibitors).[37] This test is no longer typically performed, equally its use can lead to life-threatening bradycardia (slow heart rate) which requires immediate emergency attention.[38] Production of edrophonium was discontinued in 2008.[20]
Imaging
A breast X-ray may identify widening of the mediastinum suggestive of thymoma, just computed tomography or magnetic resonance imaging (MRI) are more than sensitive means to identify thymomas and are generally washed for this reason.[39] MRI of the cranium and orbits may also exist performed to exclude compressive and inflammatory lesions of the cranial nerves and ocular muscles.[xl]
Pulmonary function test
The forced vital capacity may exist monitored at intervals to detect increasing muscular weakness. Acutely, negative inspiratory force may be used to determine adequacy of ventilation; it is performed on those individuals with MG.[41] [42]
Management
Treatment is past medication and/or surgery. Medication consists mainly of acetylcholinesterase inhibitors to directly improve muscle function and immunosuppressant drugs to reduce the autoimmune procedure.[43] Thymectomy is a surgical method to treat MG.[44]
Medication

Neostigmine, chemical structure

Azathioprine, chemical structure
Worsening may occur with medication such as fluoroquinolones, aminoglycosides, and magnesium.[45] Well-nigh 10% of people with generalized MG are considered treatment-refractory.[46] Autologous hematopoietic stem prison cell transplantation (HSCT) is sometimes used in astringent, treatment-refractory MG. Available data provide preliminary evidence that HSCT tin can exist an effective therapeutic option in carefully selected cases.[47]
Efgartigimod alfa was approved for medical use in the United states of america in Dec 2021.[48] [49] [50]
Acetylcholinesterase inhibitors
Acetylcholinesterase inhibitors can provide symptomatic do good and may non fully remove a person'due south weakness from MG.[51] While they might not fully remove all symptoms of MG, they still may allow a person the ability to perform normal daily activities.[51] Usually, acetylcholinesterase inhibitors are started at a depression dose and increased until the desired upshot is achieved. If taken 30 minutes earlier a meal, symptoms volition exist mild during eating, which is helpful for those who take difficulty swallowing due to their illness. Another medication used for MG, atropine, can reduce the muscarinic side furnishings of acetylcholinesterase inhibitors.[52] Pyridostigmine is a relatively long-interim drug (when compared to other cholinergic agonists), with a one-half-life around 4 hours with relatively few side effects.[53] Generally, it is discontinued in those who are being mechanically ventilated, as it is known to increase the amount of salivary secretions.[53] A few high-quality studies accept directly compared cholinesterase inhibitors with other treatments (or placebo); their practical benefit may be such that conducting studies in which they would exist withheld from some people would exist difficult.[43]
Immune suppressants
The steroid prednisone might besides be used to reach a amend result, simply it can lead to the worsening of symptoms for xiv days and takes 6–8 weeks to attain its maximal effectiveness.[53] Due to the myriad symptoms that steroid treatments tin can cause, it is not the preferred method of treatment.[53] Other immune suppressing medications may too be used including rituximab.[54]
Plasmapheresis and IVIG
If the myasthenia is serious (myasthenic crisis), plasmapheresis can be used to remove the putative antibodies from the circulation. Besides, intravenous immunoglobulins (IVIGs) can be used to demark the circulating antibodies. Both of these treatments accept relatively short-lived benefits, typically measured in weeks, and often are associated with high costs, which make them prohibitive; they are generally reserved for when MG requires hospitalization.[53] [55]
Surgery
As thymomas are seen in 10% of all people with the MG, they are often given a chest 10-ray and CT scan to evaluate their demand for surgical removal of their thymus glands and any cancerous tissue that may exist present.[twenty] [38] Fifty-fifty if surgery is performed to remove a thymoma, information technology mostly does not atomic number 82 to the remission of MG.[53] Surgery in the case of MG involves the removal of the thymus, although in 2013, no clear do good was indicated except in the presence of a thymoma.[56] A 2016 randomized, controlled trial, however, found some benefits.[57]
Physical measures
People with MG should be educated regarding the fluctuating nature of their symptoms, including weakness and do-induced fatigue. Exercise participation should exist encouraged with frequent rest.[15] In people with generalized MG, some show indicates a partial abode programme including grooming in diaphragmatic breathing, pursed-lip breathing, and interval-based muscle therapy may improve respiratory musculus forcefulness, chest wall mobility, respiratory pattern, and respiratory endurance.[58]
Medical imaging
In people with myasthenia gravis, older forms of iodinated dissimilarity used for medical imaging have caused an increased risk of exacerbation of the disease, but modern forms have no immediate increased take a chance.[59]
Prognosis
The prognosis of people with MG is generally good, equally is quality of life, given very adept treatment.[60] Monitoring of a person with MG is very of import, as at to the lowest degree 20% of people diagnosed with it volition experience a myasthenic crisis within two years of their diagnosis, requiring rapid medical intervention.[53] Generally, the most disabling period of MG might be years afterwards the initial diagnosis.[51] In the early 1900s, 70% of detected cases died from lung issues; now, that number is estimated to exist around 3–5%, which is attributed to increased awareness and medications to manage symptoms.[53]
Epidemiology
MG occurs in all ethnic groups and both sexes. Information technology most ordinarily affects women nether forty and people from l to 70 years old of either sex, but information technology has been known to occur at any age. Younger people rarely take thymoma. Prevalence in the Usa is estimated at between 0.5 and 20.4 cases per 100,000, with an estimated lx,000 Americans afflicted.[20] [61] Inside the United Kingdom, an estimated 15 cases of MG occur per 100,000 people.[38]
History
The first to write about MG were Thomas Willis, Samuel Wilks, Erb, and Goldflam.[xvi] The term "myasthenia gravis pseudo-paralytica" was proposed in 1895 by Jolly, a German physician.[xvi] Mary Walker treated a person with MG with physostigmine in 1934.[sixteen] Simpson and Nastuck detailed the autoimmune nature of the condition.[16] In 1973, Patrick and Lindstrom used rabbits to show that immunization with purified musculus-like acetylcholine receptors acquired the development of MG-similar symptoms.[sixteen]
Enquiry
Immunomodulating substances, such equally drugs that prevent acetylcholine receptor modulation by the immune organization, are currently being researched.[62] Some research recently has been on anti-c5 inhibitors for handling inquiry equally they are safe and used in the handling of other diseases.[63] Ephedrine seems to benefit some people more other medications, but information technology has not been properly studied equally of 2014.[nine] [64] In the laboratory, MG is mostly studied in model organisms, such as rodents. In addition, in 2015, scientists adult an in vitro functional, all-human, neuromuscular junction assay from human embryonic stem cells and somatic-muscle stem cells. After the improver of pathogenic antibodies against the acetylcholine receptor and activation of the complement system, the neuromuscular co-civilisation shows symptoms such equally weaker muscle contractions.[65]
References
- ^ a b c d e f g h i j g l m n o p q r s t u v w x "Myasthenia Gravis Fact Sheet". National Plant of Neurological Disorders and Stroke.
- ^ Kahan Due south (2005). In a Page: Neurology. Lippincott Williams & Wilkins. p. 118. ISBN978-1-4051-0432-half dozen. Archived from the original on eight September 2017.
- ^ a b Kaminski HJ (2009). Myasthenia Gravis and Related Disorders (2 ed.). Springer Scientific discipline & Business Media. p. 72. ISBN978-i-59745-156-vii. Archived from the original on eight September 2017.
- ^ a b Adams JG (2012). Emergency Medicine: Clinical Essentials (2 ed.). Elsevier Wellness Sciences. p. 844. ISBN978-1-4557-3394-i. Archived from the original on 8 September 2017.
- ^ Immature C, McGill SC. Rituximab for the Treatment of Myasthenia Gravis: A 2021 Update [Cyberspace]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2021 Apr. Available from: https://world wide web.ncbi.nlm.nih.gov/books/NBK571915/
- ^ Jayam Trouth A, Dabi A, Solieman N, Kurukumbi M, Kalyanam J� Myasthenia gravis: a review� Autoimmune Dis. 2012;2012:874680-874680
- ^ a b Phillips WD, Vincent A (1 Jan 2016). "Pathogenesis of myasthenia gravis: update on disease types, models, and mechanisms". F1000Research. v: 1513. doi:10.12688/f1000research.8206.1. PMC4926737. PMID 27408701.
- ^ Kandel Eastward, Schwartz J, Jessel T, Siegelbaum S, Hudspeth A (2012). Principles of Neural Science (5 ed.). pp. 318–319.
- ^ a b Vrinten C, van der Zwaag AM, Weinreich SS, Scholten RJ, Verschuuren JJ (December 2014). "Ephedrine for myasthenia gravis, neonatal myasthenia and the congenital myasthenic syndromes". The Cochrane Database of Systematic Reviews. 12 (12): CD010028. doi:10.1002/14651858.CD010028.pub2. PMC7387729. PMID 25515947.
- ^ Godoy DA, Mello LJ, Masotti L, Di Napoli M (September 2013). "The myasthenic patient in crunch: an update of the management in Neurointensive Care Unit of measurement". Arquivos de Neuro-Psiquiatria. 71 (9A): 627–39. doi:10.1590/0004-282X20130108. PMID 24141444.
- ^ a b McGrogan A, Sneddon S, de Vries CS (2010). "The incidence of myasthenia gravis: a systematic literature review". Neuroepidemiology. 34 (3): 171–183. doi:ten.1159/000279334. PMID 20130418. S2CID 34447321.
- ^ Ehrlich A, Schroeder CL (2014). Introduction to Medical Terminology. Cengage Learning. p. 87. ISBN978-1-133-95174-two. Archived from the original on eight September 2017.
- ^ a b c d e f g h i j Engel AG (2012). Myasthenia Gravis and Myasthenic Disorders (2nd ed.). Oxford University Press, Usa. pp. 109–110. ISBN978-0-xix-973867-0. Archived from the original on 8 September 2017.
- ^ a b c d e Scully C (2014). Scully'southward Medical Issues in Dentistry. Elsevier Health Sciences UK. ISBN978-0-7020-5963-vi. Archived from the original on viii September 2017.
- ^ a b Myasthenia Gravis at eMedicine
- ^ a b c d due east f g h Nair AG, Patil-Chhablani P, Venkatramani DV, Gandhi RA (October 2014). "Ocular myasthenia gravis: a review". Indian Journal of Ophthalmology. 62 (10): 985–991. doi:ten.4103/0301-4738.145987. PMC4278125. PMID 25449931.
- ^ a b c d e f yard Scherer 1000, Bedlack RS, Simel DL (April 2005). "Does this patient have myasthenia gravis?". JAMA. 293 (15): 1906–1914. doi:ten.1001/jama.293.fifteen.1906. PMID 15840866.
- ^ a b Rajendran A; Sundaram S (2014). Shafer's Textbook of Oral Pathology (7th ed.). Elsevier Wellness Sciences APAC. p. 867. ISBN978-81-312-3800-4. Archived from the original on 2 April 2017.
- ^ MedlinePlus Encyclopedia: Myasthenia gravis
- ^ a b c d e Marx JA (2014). Rosen's emergency medicine: concepts and clinical practice (8th ed.). Philadelphia: Elsevier/Saunders. pp. 1441–1444. ISBN978-1-4557-0605-1.
- ^ "Myasthenia gravis". Genetics Domicile Reference. Archived from the original on xi July 2015. Retrieved 10 July 2015.
- ^ Sinmaz Due north, Nguyen T, Tea F, Dale RC, Brilot F (August 2016). "Mapping autoantigen epitopes: molecular insights into autoantibody-associated disorders of the nervous system". Journal of Neuroinflammation. xiii (1): 219. doi:x.1186/s12974-016-0678-4. PMC5006540. PMID 27577085.
- ^ Sathasivam S (Jan 2014). "Diagnosis and management of myasthenia gravis". Progress in Neurology and Psychiatry. xviii (1): half dozen–14. doi:ten.1002/pnp.315. S2CID 115659064.
- ^ "Myasthenia Gravis". PubMed Wellness. Bethesda, MD: National Library of Medicine. Archived from the original on eighteen October 2016. Retrieved ix July 2015.
- ^ "Myasthenia Gravis Fact Sheet". www.ninds.nih.gov. National Institute of Neurological Disorders and Stroke (NINDS). Archived from the original on 11 July 2015. Retrieved 10 July 2015.
- ^ a b c Varner K (June 2013). "Myasthenia gravis and pregnancy". Clinical Obstetrics and Gynecology. 56 (2): 372–81. doi:10.1097/GRF.0b013e31828e92c0. PMID 23563874.
- ^ Téllez-Zenteno JF, Hernández-Ronquillo Fifty, Salinas V, Estanol B, da Silva O (November 2004). "Myasthenia gravis and pregnancy: clinical implications and neonatal effect". BMC Musculoskeletal Disorders. five (1): 42. doi:10.1186/1471-2474-five-42. PMC534111. PMID 15546494.
- ^ a b c Warrell DA, Cox TM, et al. (2003). Oxford Textbook of Medicine. Vol. 3 (Fourth ed.). Oxford. p. 1170. ISBN978-0-19-852787-ix.
- ^ Rudd 1000, Kocisko D (2013). Pediatric Nursing: The Critical Components of Nursing Intendance. F.A. Davis. ISBN978-0-8036-4053-5. Archived from the original on iii June 2016.
- ^ Engel AG, Shen XM, Selcen D, Sine SM (April 2015). "Built myasthenic syndromes: pathogenesis, diagnosis, and handling". The Lancet. Neurology. 14 (four): 420–434. doi:10.1016/S1474-4422(fourteen)70201-7. PMC4520251. PMID 25792100.
- ^ "Congenital Myasthenia Data Page: National Institute of Neurological Disorders and Stroke (NINDS)". www.ninds.nih.gov. Archived from the original on 12 July 2015. Retrieved 11 July 2015.
- ^ Wolfe GI, Barohn RJ (2009). "Myasthenia Gravis: Nomenclature and Outcome Measurements". Myasthenia Gravis and Related Disorders. pp. 293–302. doi:10.1007/978-1-59745-156-7_18. ISBN978-1-58829-852-2.
- ^ Leite MI, Jacob S, Viegas S, Cossins J, Clover Fifty, Morgan BP, et al. (July 2008). "IgG1 antibodies to acetylcholine receptors in 'seronegative' myasthenia gravis". Brain. 131 (Pt 7): 1940–52. doi:10.1093/brain/awn092. PMC2442426. PMID 18515870.
- ^ MedlinePlus Encyclopedia: Lambert-Eaton syndrome
- ^ Selvan VA (January 2011). "Single-fiber EMG: A review". Annals of Indian Academy of Neurology. 14 (ane): 64–67. doi:10.4103/0972-2327.78058. PMC3108086. PMID 21654930.
- ^ Kearsey C, Fernando P, D'Costa D, Ferdinand P (June 2010). "The use of the ice pack test in myasthenia gravis". JRSM Short Reports. i (1): 14. doi:10.1258/shorts.2009.090037. PMC2984327. PMID 21103106.
- ^ MedlinePlus Encyclopedia: Tensilon examination
- ^ a b c Spillane J, Higham Eastward, Kullmann DM (Dec 2012). "Myasthenia gravis". BMJ. 345 (dec21 3): e8497. doi:10.1136/bmj.e8497. PMID 23261848. S2CID 13911967.
- ^ de Kraker M, Kluin J, Renken N, Maat AP, Bogers AJ (June 2005). "CT and myasthenia gravis: correlation betwixt mediastinal imaging and histopathological findings". Interactive Cardiovascular and Thoracic Surgery. 4 (3): 267–271. doi:ten.1510/icvts.2004.097246. PMID 17670406.
- ^ Allan H. Ropper, Robert H. Brown Adams and Victor's Principles of Neurology McGraw-Hill Professional person; 8 edition (2005)
- ^ MedlinePlus Encyclopedia: Pulmonary office tests
- ^ Emergent Management of Myasthenia Gravis at eMedicine
- ^ a b Mehndiratta MM, Pandey S, Kuntzer T (October 2014). "Acetylcholinesterase inhibitor handling for myasthenia gravis". The Cochrane Database of Systematic Reviews (10): CD006986. doi:ten.1002/14651858.CD006986.pub3. PMC7390275. PMID 25310725.
- ^ Gronseth GS, Barohn RJ (July 2000). "Practice parameter: thymectomy for autoimmune myasthenia gravis (an evidence-based review): study of the Quality Standards Subcommittee of the American University of Neurology". Neurology. 55 (1): seven–15. doi:10.1212/wnl.55.ane.vii. PMID 10891896.
- ^ Mehrizi M, Fontem RF, Gearhart TR, Pascuzzi RM (August 2012). "Medications and Myasthenia Gravis (A Reference for Health Care Professionals)" (PDF). S2CID 9640884.
- ^ Suh J, Goldstein JM, Nowak RJ (June 2013). "Clinical characteristics of refractory myasthenia gravis patients". The Yale Periodical of Biology and Medicine. 86 (2): 255–60. PMC3670444. PMID 23766745.
- ^ Burman J, Tolf A, Hägglund H, Askmark H (February 2018). "Autologous haematopoietic stem jail cell transplantation for neurological diseases". Periodical of Neurology, Neurosurgery, and Psychiatry. 89 (2): 147–155. doi:ten.1136/jnnp-2017-316271. PMC5800332. PMID 28866625.
- ^ "FDA Approves New Treatment for Myasthenia Gravis". U.Due south. Nutrient and Drug Administration (FDA) (Press release). 17 December 2021. Retrieved 21 Dec 2021.
 This article incorporates text from this source, which is in the public domain .
This article incorporates text from this source, which is in the public domain . - ^ "argenx Announces U.Due south. Food and Drug Assistants (FDA) Approval of Vyvgart (efgartigimod alfa-fcab) in Generalized Myasthenia Gravis". Argenx (Press release). 17 December 2021. Retrieved 21 December 2021.
- ^ "argenx Announces U.S. Food and Drug Assistants (FDA) Approval of Vyvgart (efgartigimod alfa-fcab) in Generalized Myasthenia Gravis" (Press release). Argenx. 17 December 2021. Retrieved 21 December 2021 – via Business Wire.
- ^ a b c Mehndiratta MM, Pandey S, Kuntzer T (Oct 2014). "Acetylcholinesterase inhibitor treatment for myasthenia gravis". The Cochrane Database of Systematic Reviews (10): CD006986. doi:ten.1002/14651858.CD006986.pub3. PMC7390275. PMID 25310725.
- ^ "Atropine – Myasthenia-gravis medicines and drugs". NHS Choices. 2014. Archived from the original on 12 July 2015. Retrieved 11 July 2015.
- ^ a b c d e f g h Kumar V, Kaminski HJ (February 2011). "Handling of myasthenia gravis". Electric current Neurology and Neuroscience Reports. 11 (1): 89–96. doi:10.1007/s11910-010-0151-1. PMID 20927659. S2CID 41052495.
- ^ Tandan R, Hehir MK, Waheed W, Howard DB (August 2017). "Rituximab treatment of myasthenia gravis: A systematic review". Muscle & Nervus. 56 (two): 185–196. doi:10.1002/mus.25597. PMID 28164324. S2CID 19504332.
- ^ Juel VC (March 2004). "Myasthenia gravis: management of myasthenic crisis and perioperative care". Seminars in Neurology. 24 (one): 75–81. doi:10.1055/s-2004-829595. PMID 15229794.
- ^ Cea G, Benatar M, Verdugo RJ, Salinas RA (October 2013). "Thymectomy for not-thymomatous myasthenia gravis". The Cochrane Database of Systematic Reviews (10): CD008111. doi:10.1002/14651858.CD008111.pub2. PMID 24122674.
- ^ Wolfe GI, Kaminski HJ, Aban IB, Minisman G, Kuo HC, Marx A, et al. (August 2016). "Randomized Trial of Thymectomy in Myasthenia Gravis". The New England Journal of Medicine. 375 (6): 511–522. doi:10.1056/NEJMoa1602489. hdl:2318/1601939. PMC5189669. PMID 27509100.
- ^ Cup EH, Pieterse AJ, 10 Broek-Pastoor JM, Munneke M, van Engelen BG, Hendricks HT, van der Wilt GJ, Oostendorp RA (November 2007). "Practice therapy and other types of physical therapy for patients with neuromuscular diseases: a systematic review". Archives of Physical Medicine and Rehabilitation. 88 (eleven): 1452–1464. doi:x.1016/j.apmr.2007.07.024. PMID 17964887.
- ^ Mehrizi K, Pascuzzi RM (September 2014). "Complications of radiologic dissimilarity in patients with myasthenia gravis". Musculus & Nerve. 50 (3): 443–4. doi:ten.1002/mus.24254. PMID 24677227. S2CID 206295540.
- ^ Sieb JP (March 2014). "Myasthenia gravis: an update for the clinician". Clinical and Experimental Immunology. 175 (iii): 408–418. doi:10.1111/cei.12217. PMC3927901. PMID 24117026.
- ^ Cea G, Benatar M, Verdugo RJ, Salinas RA (Oct 2013). "Thymectomy for non-thymomatous myasthenia gravis". The Cochrane Database of Systematic Reviews (10): CD008111. doi:10.1002/14651858.CD008111.pub2. PMID 24122674.
- ^ Losen M, Martínez-Martínez P, Phernambucq M, Schuurman J, Parren Pw, De Baets MH (2008). "Treatment of myasthenia gravis by preventing acetylcholine receptor modulation". Annals of the New York University of Sciences. 1132 (one): 174–179. Bibcode:2008NYASA1132..174L. doi:10.1196/annals.1405.034. PMID 18567867. S2CID 3206109.
- ^ Conti-Fine BM, Milani Thou, Kaminski HJ (November 2006). "Myasthenia gravis: by, present, and future". The Journal of Clinical Investigation. 116 (11): 2843–2854. doi:ten.1172/JCI29894. PMC1626141. PMID 17080188.
- ^ Vrinten C, van der Zwaag AM, Weinreich SS, Scholten RJ, Verschuuren JJ (December 2014). "Ephedrine for myasthenia gravis, neonatal myasthenia and the congenital myasthenic syndromes". The Cochrane Database of Systematic Reviews. 12 (12): CD010028. doi:10.1002/14651858.CD010028.pub2. PMC7387729. PMID 25515947.
- ^ Steinbeck JA, Jaiswal MK, Calder EL, Kishinevsky South, Weishaupt A, Toyka KV, Goldstein PA, Studer L (Jan 2016). "Functional Connectivity under Optogenetic Control Allows Modeling of Human Neuromuscular Disease". Cell Stem Jail cell. eighteen (1): 134–143. doi:10.1016/j.stalk.2015.10.002. PMC4707991. PMID 26549107.
Further reading
- Zhang Z, Guo J, Su M, Li J, Wu H, Xie X (17 November 2014). "Evaluation of the quality of guidelines for myasthenia gravis with the Agree Ii instrument". PLOS ONE. nine (11): e111796. Bibcode:2014PLoSO...9k1796Z. doi:10.1371/journal.pone.0111796. PMC4234220. PMID 25402504.
- "NCBI – Diagnostic". www.ncbi.nlm.nih.gov . Retrieved 11 July 2015.
![]() This page was concluding edited on 13 March 2022, at 23:58
This page was concluding edited on 13 March 2022, at 23:58
davidsonshypeation.blogspot.com
Source: https://wiki2.org/en/Myasthenia_gravis
0 Response to "How Do You Know Youre Dying From Myasthenia Gravis"
Post a Comment